Independent Medical Practice Challenges: Why Remaining Independent is So Hard

This is part 2 of a three-part series on the importance of independent specialty practices in America. Part 1 explains why independent practices are foundational to healthcare, this part describes the challenges of independence, and Part 3 explains why the right partner can make all the difference.
Independent Medical Practice Challenges: Why Remaining Independent is So Hard
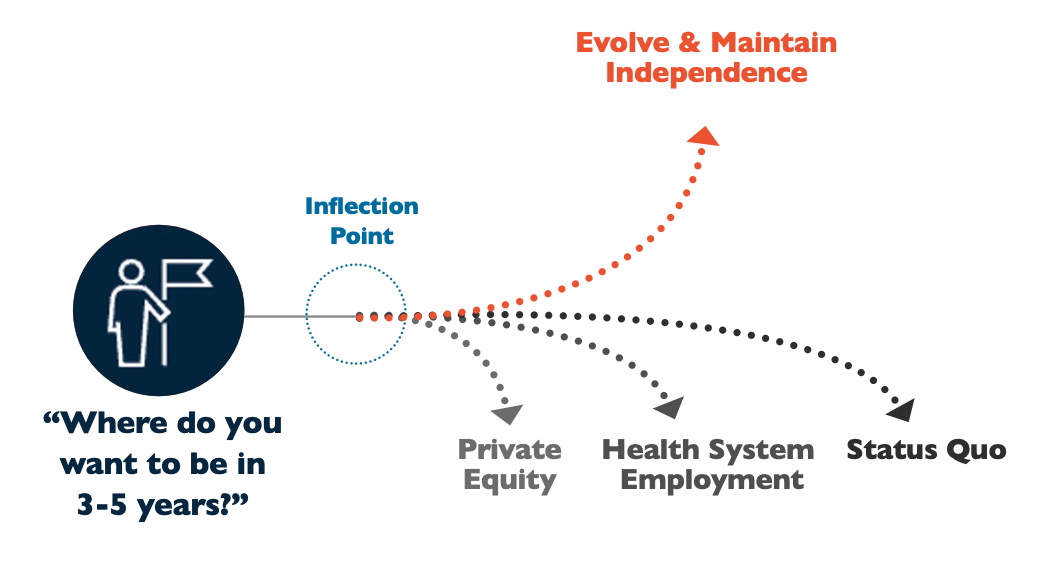
The biggest conundrum of staying independent is that the rate of changes in reimbursement, regulatory, reporting, and other administrative burdens are so great that it’s nearly impossible to run the business side of a practice while still maintaining your day job as an actual doctor. You don’t have the time or funds to build a team of policy experts or become one yourself independently, but at the same time, you can’t afford to ignore the constantly changing policy and trends that impact your bottom line.
It’s Hard, but Remaining Independent is Possible
Independent Medical Practice Challenges
It’s clear that independent specialty practices are needed to keep healthcare costs down and continue to provide high-quality patient care — but practices have many hurdles in their way:
- Navigating regulatory compliance and payor guidelines
- Finding and retaining quality staff
- Struggling with outdated technology
- Satisfying increasing patient expectations
- Transitioning to new care models
- …just to name a few.
There’s Not Just One Independent Medical Practice Challenge to Deal With
Independent practices must combine new business processes and technology to address current challenges and stay ahead of new ones.
Successful independent practices are adopting key strategies, such as:
- Investing in modern technologies to improve patient experience.
- Diversifying offerings and adding ancillary services to expand care.
- Monitoring health outcomes data to boost business performance.
- Adopting tools to track KPIs and strengthen financial management.
- Staying up to date on regulations and value-based care programs to stay relevant.
- Exploring alternative payment models to maximize revenue.
- Building collaborative networks with other providers to widen referrals.
- Focusing on patient-centered care to improve patient retention.
- Deploying care pathways to ensure patients get the care they need, when and where they need it.
93% of independent physicians report feeling that their job holds valuable advantages compared to their employed peers.
It is Many, Complicated Interconnected Things
Independent private practices face numerous obstacles, and practice owners are pulled in a million directions trying to fix them. Many of these challenges are linked, but tracing those links to find common solutions feels overwhelming.
Getting ahead requires a holistic approach to evolve into a modern, value-based practice — but how do you start?
Independent Medical Practice Challenge Example: Specialty Referral Flows
What would happen to your specialty practice if the number of referrals you received dropped by a third? How about by two-thirds?
 This isn’t a hypothetical question — your stellar record in patient treatments and longstanding personal and professional relationships with local primary care physicians (PCPs) might not be enough to protect your future referrals.
This isn’t a hypothetical question — your stellar record in patient treatments and longstanding personal and professional relationships with local primary care physicians (PCPs) might not be enough to protect your future referrals.
Payers are holding PCPs’ feet to the fire when it comes to the total cost of care. That includes the cost of your care when they refer one of their patients to your practice. As a result, PCPs are becoming more selective in their specialist referrals. What’s more, payers are increasingly evaluating specialists of all sorts and grading them based on costs and outcomes.
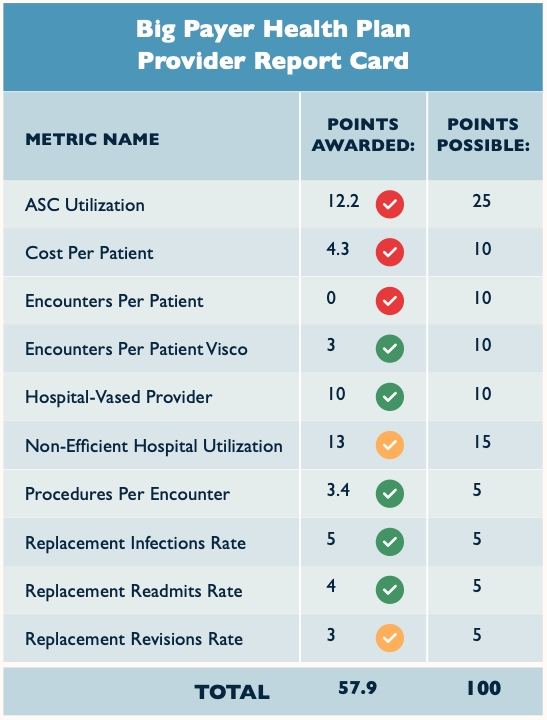
At least some of the payers in your area are providing a report card to your referring PCPs in an effort to influence where they refer. This includes cost/quality metrics like ASC utilization rates, cost per patient, encounters per patient, procedures per encounter, replacement readmits, etc. Increasingly, these report cards will matter when it comes to the volume of referrals that your practice sees.
Of course, this is hardly the first or only time that payers are reducing your work as a physician into a few simplistic numbers. As a result, your report card may or may not look good, and you won’t have another opportunity for further explanation. You need to be aware of how
your practice is being evaluated. Then, you need to be ready to contextualize those numbers with population or disease state statistics. Lastly, you should take a step back and look at the overall cost of care and how your practice fits into it.
Do you know what payers are saying about you to your referring PCPs?
Getting Holistic About the Cost of Care
Many physicians are uncomfortable discussing the cost of care, but it’s a topic that isn’t going away. Moreover, it’s not necessarily the zero-sum conversation that you might fear.
Chances are good that your fees are only a small part of any given patient’s total cost of care. For instance, a surgeon may charge a few thousand dollars for minor surgery, but the home healthcare company may charge tens of thousands for at-home care and physical therapy afterward. So, if you allow payers to focus on just the surgery itself as a cost driver, you’re missing out on two huge opportunities to advocate for yourself. First, to be rewarded for delivering quality care at a lower cost and, second, for providing higher quality care to your patients.
One way to take advantage of that opportunity is to position your specialty practice to exert more control on the clinical pathways for your patients both before and after they visit your practice. A clinically integrated network like this ensures that your patients receive the best care and will, not incidentally, reduce the overall care cost through less unnecessary testing, complications, or readmissions.
Taking a proactive approach to referrals and cost of care is necessary for practices looking to thrive as independent entities in the decades to come.

That Sounds…Complicated
It is. And there’s no cookie-cutter one-size-fits-all pathway to success. Every market and every practice requires a slightly different approach.
However, there are some commonalities. You’ll need to harness specialized tools to gather and present outcomes and cost-of-care data. Communication throughout the continuum of care is critical and requires significant electronic interoperability between PCPs, specialists, and post-acute providers. And, of course, you’ll need to reach out to your colleagues to discuss these challenges. Even ones that you’ve been working with for decades. Most of all, physicians need to be willing to avoid a head-in-the-sand approach and tackle these challenges head-on.
There’s no easy path to clinical independence and financial success, but it’s not a journey that you need to take alone.



.png?width=500&height=380&name=Banner%20Providers%20(1).png)
.png?width=500&height=380&name=Banner%20Providers%20(2).png)
.png?width=500&height=380&name=Banner%20Providers%20(4).png)